Understanding the IVF Lab Process: What Happens Between Egg Retrieval and Embryo Transfer?
For patients undergoing in vitro fertilization (IVF) at Indiana Fertility Institute, one of the most fascinating—and often mysterious—parts of the journey takes place behind the scenes, in the lab. Beginning with the egg retrieval, your fertility team goes to work on a series of intricate, carefully timed steps that will prepare your embryos for transfer. Here, we’ll walk you through each step of the lab process to give you a clear picture of what’s happening and how every stage is designed to help maximize the chances of success.
Step 1: Egg Retrieval
Egg retrieval is the first hands-on step in the IVF lab process, where mature eggs are carefully removed from your ovaries. This procedure takes place under light sedation, ensuring comfort while your physician uses ultrasound guidance to aspirate fluid from each ovarian follicle. The follicular fluid is immediately sent to our IVF lab for the eggs to be identified and prepared for the next step in the process, fertilization.
Step 2: Sperm Collection and Preparation
After egg retrieval, a sperm sample is collected, either from a partner or a donor. The sperm sample is prepared in the lab through a process called sperm washing, which separates motile sperm from the rest of the sample. The goal here is to ensure most ideal sperm present in the provided sample are used for insemination and fertilization, maximizing the chances of successful embryo development.
Step 3: Insemination and Fertilization – Conventional Insemination or ICSI?
Once the mature eggs and the prepared sperm are ready, it’s time for insemination and fertilization. In the lab, this may happen through two main methods:
-
Conventional Insemination: In conventional insemination, the sperm and eggs are combined in a petri dish, allowing the sperm to fertilize the egg through their own interactions. This approach requires a large number of healthy, motile sperm.
-
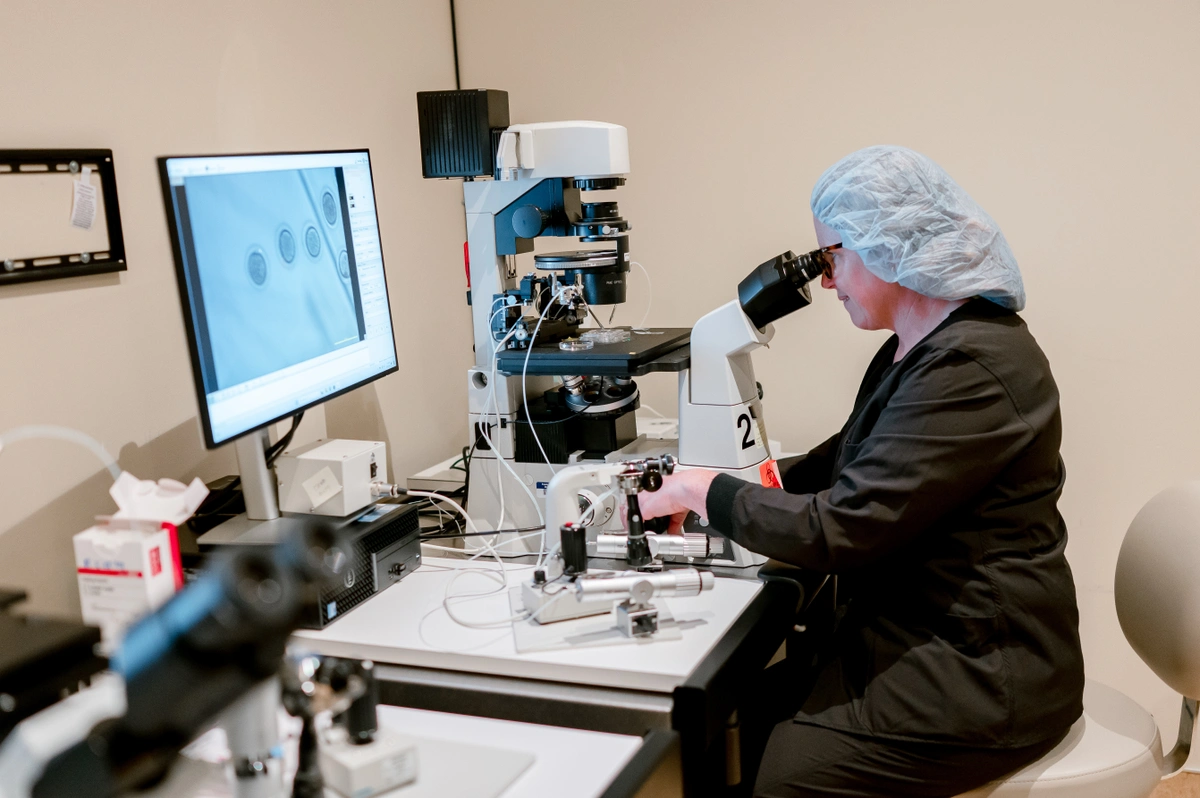
Intracytoplasmic Sperm Injection (ICSI): For patients facing male infertility factors or in cases with a limited number of sperm, the ICSI method is often preferred. With ICSI, a single sperm is directly injected into each mature egg using a micropipette. This process bypasses the conventional insemination process and has high success rates in situations where male infertility factors are a concern.
Step 4: Embryo Culture and Development
After fertilization, the embryos are placed in a controlled incubator where they begin to grow and divide. This process is called embryo culture, and it typically lasts 5 to 7 days. The lab environment simulates the conditions within the human body as closely as possible, keeping embryos in carefully monitored settings to support optimal growth.
During embryo culture, our embryologists monitor each embryo’s development, observing its growth from a single cell into a multi-cell structure. By day 3, the embryo typically has around 8 cells. If it continues developing well, it reaches the blastocyst stage by days 5 to 7. Blastocyst-stage embryos generally have a higher chance of successful implantation, which is why many clinics prefer to transfer embryos at this stage.
Step 5: Embryo Grading
As embryos develop, they are graded based on appearance and growth characteristics. Embryo grading helps embryologists identify the embryos with the best chance for a successful pregnancy. Factors like cell number, symmetry, and fragmentation are all taken into consideration during grading. While grading isn’t an absolute predictor, it provides helpful insights to guide which embryos may be best for transfer or freezing.
Step 6: Genetic Testing (Optional)
Some patients may choose to have preimplantation genetic testing (PGT) performed on their embryos. PGT is an advanced procedure that screens embryos for chromosomal abnormalities or specific genetic disorders. For patients with a known family history of genetic conditions or those experiencing recurrent miscarriages, genetic testing can be a valuable step in increasing the likelihood of a healthy pregnancy. PGT requires biopsy of cells from the embryo. The biopsy of cells is typically done on days 5, 6 and/or 7. The embryos are frozen after biopsy to await PGT results.
Step 7: Preparing for Embryo Transfer
While the lab team is hard at work on embryo development, your fertility team is preparing you for the embryo transfer. This involves ensuring that the uterine lining is optimal for implantation, sometimes with medications or other supportive treatments. Your doctor and care team will guide you through any steps you need to follow at this stage to get ready for transfer day.
Step 8: Embryo Transfer
Embryo transfer is a relatively simple procedure that typically requires no sedation. Using ultrasound guidance, your doctor will place an embryo directly into your uterus through a thin catheter. For many patients, this moment is the culmination of months or years of effort—and it’s often accompanied by hope and excitement. Following the transfer, a brief rest period is usually recommended.
Step 9: The Waiting Period
After the transfer, it’s time for the two-week wait before you can take a pregnancy test. During this time, many patients are advised to avoid intense physical activity, practice self-care, and stay as relaxed as possible. Your doctor will provide specific guidance on what to do—and what to avoid—during this time.
Freezing Embryos for Future Use
If non-transferred embryos are of acceptable quality, they can be frozen and stored for future use through a process called cryopreservation. This is a great option for those considering additional children or those who want to maximize their chances for future cycles without repeating the entire IVF process. Frozen embryos can remain viable for years, providing peace of mind and flexibility in planning your family.
Conclusion: Every Step Counts in the IVF Lab Process
Every detail of the IVF lab process is designed with precision, care, and expertise. From the fertilization stage to embryo grading, the entire lab process is focused on providing the highest chance of success for each patient. While much of this process happens behind the scenes, we hope this overview gives you a clearer understanding of what’s involved.
If you have questions about any part of the IVF process, don’t hesitate to reach out to our team. We’re here to support you at every stage and ensure that you feel confident and informed throughout your fertility journey!

